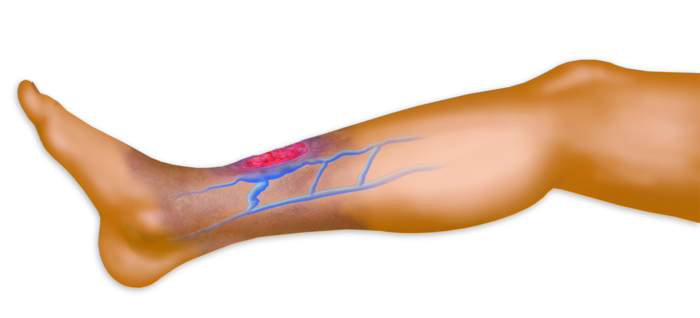
 Venous ulcer, also called stasis ulcer, is the most common type of ulceration that occurs on the legs and feet. According to varicose vein doctors in Montgomery County, approximately 70-80% of leg ulcers are venous ulcers, and they affect almost 1% of the U.S. population. Venous ulcers are usually recurrent and slow to heal. In fact, an open venous ulcer can continue for a few weeks to several years. The most common risk factors for venous ulcer include aging, obesity and overweight, pre-existing leg injuries, deep venous thrombosis (blood clots) and phlebitis (inflammation of the vein wall).
Venous ulcer, also called stasis ulcer, is the most common type of ulceration that occurs on the legs and feet. According to varicose vein doctors in Montgomery County, approximately 70-80% of leg ulcers are venous ulcers, and they affect almost 1% of the U.S. population. Venous ulcers are usually recurrent and slow to heal. In fact, an open venous ulcer can continue for a few weeks to several years. The most common risk factors for venous ulcer include aging, obesity and overweight, pre-existing leg injuries, deep venous thrombosis (blood clots) and phlebitis (inflammation of the vein wall).
Severe complications can develop if ulcers are not treated in a timely manner. These consequences can include cellulitis (infection of the skin), osteomyelitis (infection of the bones) and unpleasant skin changes such as dermatitis, skin thickening and permanent discoloration of the skin. Advanced cases of venous ulcer can result in inflammation and edema and may be very large or may take years to heal.
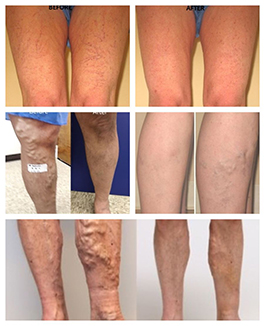
These types of ulcers are normally located just above the ankle, usually on the inside of the leg. In the past, most venous ulcers were only treated with specialized dressings and the use of prescription-grade compression hose, compression wraps or a gauze wrap with paste called an Unna’s boot, that may leave patients vulnerable to slow healing or recurrence.
Today, conservative treatment options for venous ulcers include leg elevation, compression therapy, dressings and therapeutic medications. Surgical management may be recommended for ulcers that are large, slow healing or do not respond to conservative measures.
Venous Health Centers, a top vein center in Montgomery County, provides expert vein consultation and duplex venous ultrasound to accurately diagnose the underlying cause of venous ulcers. Based on the non-invasive venous ultrasound, our Washington DC vein specialist offers treatment of the underlying vein disease with a range of minimally invasive endovenous thermal ablation procedures. These treatments have been shown to reduce healing time by as much as 50% and to reduce the likelihood of recurrence.