Venous Disease
Q: What are varicose veins?
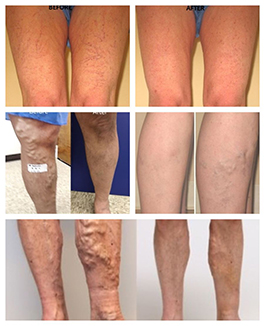
A: Varicose veins are raised, enlarged veins. Which usually appear on the skin surface and can cause the leg to swell, burn, fatigue, itch, or ache. In severe cases, they can bleed, lead to skin discoloration or cause ulcers.
Normal vein valves close after blood travels up the vein, preventing blood from moving backwards (refluxing) down the vein. Varicose veins form when valves in the vein fail (become incompetent). Valves become incompetent for a variety of reasons, including heredity, trauma, and pregnancy. Once a valve becomes incompetent, the vein below the valve is exposed to higher pressure and becomes dilated. This causes other valves to fail and other veins to dilate.
Q: What are symptoms of varicose veins?
A: Leg pain, aching, or cramping
- Burning or itching
- Restless legs
- Leg or ankle swelling
- Heavy feeling in legs or fatigue
- Skin discolorations or texture changes
- Open wounds or sores
Q: Is venous disease a hereditary disorder?
A: In a study involving 134 families, the risk of developing varicose veins was: 89% if both parents had varicose veins, 47% if one parent had varicose veins and 20% if neither parent had varicose veins.
Q: Is this loss of a vein a problem?
A: No. Minimally invasive procedures act to seal a faulty diseased vein. The diseased vein is dysfunctional and is allowing blood to flow backward and pool in your leg. So leaving it open will only make things worse. Treatment of the unhealthy or diseased veins almost always results in improved blood flow in the overall circulatory system. Once the diseased vein is closed, other healthy veins will take over and carry blood flow from the leg, re-establishing a more normal flow.
Q: How are varicose veins diagnosed?
A: Along with your initial physical exam further testing is often required which includes duplex Doppler ultrasound exams of the legs. This non-invasive painless test uses sound waves to evaluate the function of the valves in the veins of the leg. This test is very important in diagnosis, and can improve the effectiveness of any treatment.
Q: What happens if I do not get the treatment?
A: Venous reflux disease, or varicose veins, is a progressive condition that only gets worse over time. This may lead to additional varicose veins and in some cases swelling and skin discoloration and texture changes, or venous ulcer above the ankle.
Q: Which doctor treats varicose veins?
A: There is a newer physician speciality called Phlebology which focuses on vein diseases. The American College of Phlebology provides board certification and speciality training. Dr. Rana has both American College of Phlebology accredited fellowship training and Board Certification in venous and lymphatic medicine.
Minimally Invasive Procedures
Q: How does the procedure actually work?
A: A thin catheter is inserted via a tiny entry point through the skin (like an I.V. line) usually near the knee. After administering local anesthesia, heat energy is then delivered to seal the faulty vein closed. The catheter is withdrawn at the end of procedure. Normal daily activities can usually be resumed, and in fact we encourage patients to plan on taking a trip to the mall afterwards to do some walking and some shopping!
Q: What are the alternatives to minimally invasive endovenous treatment of varicose veins?
A: Surgery (called ‘Ligation & Stripping’) is the traditional treatment, but it can be quite painful and often has a long recovery time. It is performed in a hospital, involves general anesthesia, leaves a scar, and has a fairly high recurrence rate (on average 10-25%).
Sclerotherapy has been used by some as an alternative but is generally only well suited for the smaller size spider or reticular veins.
Q: Is the minimally invasive closure procedure painful?
A: Patients report little, if any, pain during the endovenous procedures. The doctor will give you local anesthesia to numb the treatment areas.
Q: What are medical grade compression stockings?
A: Compression stockings or socks are now available in a variety of styles, textures and colors for both men and women. Graduated compression prevents blood from pooling in the leg veins, thereby helping overall circulation. Compression is greatest at the ankle and gradually decreases up the leg. They compress the lower leg and decrease the swelling and the other symptoms of varicose veins. They come in various strengths and are fitted by a trained technician. They are worn as preventive care, during the treatment of varicose veins and after treatment to assist in the healing process, and to maximize results of therapy and reduce risk of deep vein thrombosis.
Q: What is the advantage of treating varicose veins by minimally invasive procedures?
A: Minimally invasive is not an open surgical procedure and is performed in an outpatient office setting.
No downtime. Most patients resume normal activities immediately. Fast recovery.
No general anesthesia; only local anesthesia.
Little to no scarring.
Relief of symptoms (but often gradual).
Q: How long does the procedure take?
A: The procedure typically takes 25-30 minutes, though patients might spend 45-60 minutes in our office due to normal pre and post treatment procedures.
Q: How soon can I return to work or normal activities?
A: The patient is ambulatory immediately after the treatement and ready to resume normal activities. Normal activities can typically be resumed within a day. Following treatment, the doctor may recommend refraining from very strenuous leg exercises for one week or heavy lifting.
Spider Veins
Q: What are spider veins?
A: Spider veins are visible on the surface of the skin as small red, purple, or blue lines and are often associated with underlying varicose veins. They may look like a series of lines, tree branches or web-like shape. Though smaller than most varicose veins, spider veins are often darker and more noticeable.
Spider veins are most commonly found on the thighs, calves, or ankles, where they become a cosmetic concern. They can cause symptoms such as tenderness, itchiness, heaviness and cramps.
Although many patients are bothered by the way they look, they can also be an indication of more serious underlying vein disease. It is important to treat underlying unhealthy veins early to halt the progression of the vein disease and to prevent complications such as edema, skin discoloration, venous ulcer or increased risk of vein thrombosis (clots).
Certain factors contribute to the development of spider veins including heredity, pregnancy, hormonal factors, weight gain, trauma, and occupations or activities that require prolonged sitting or standing.
Q: What type of sclerotherapy results for spider veins can I expect?
A: Most spider veins will lighten and/or disappear. Upon the first treatment, 70%-75% of spider veins will fade or disappear. Sclerotherapy does not yield perfect results. Significant improvement usually occurs, but perfection is rarely achieved. As long as you expect significant improvement and not perfection, you should be satisfied. Full results may not be seen for 8-12 weeks.
Q: What are spider veins?
A: Spider veins are small red, blue or purple veins that appear on the surface of the thighs, calves and ankles.They may appear as a group of veins radiating outward from a central point, in a pattern that resembles branches on a tree or they may appear as thin separate lines. Spider veins may be isolated or associated with “feeder” veins.
They can also be associated with larger underlying varicose veins. Certain factors contribute to the development of spider veins, including heredity, pregnancy, hormonal factors, weight gain, and occupations or activities that require prolonged sitting or standing, and trauma.
Q: What is sclerotherapy?
A: Sclerotherapy is the standard, preferred treatment for small, uncomplicated spider veins. Sclerotherapy is a quick procedure with no downtime. A sclerosing solution is injected into the vein, using a tiny needle as fine as a human hair. The vein becomes irritated; collapses and is gradually absorbed by the body. Most patients agree that sclerotherapy is much less painful then laser treatment. In the past, the pain associated with sclerotherapy was not the injection but rather due to the solutions used. With newer medications, there is less pain caused by the solutions. The patient wears compression stockings after the sclerotherapy and is ambulatory immediately after the treatment
Q: What is the cost of vein treatment?
A: Medically necessary procedures like minimally invasive endovenous radiofrequency ablation, endovenous laser ablation, Micro-phlebectomy, ultrasound-guided sclerotherapy, and non-invasive Doppler venous ultrasound are covered by most insurances including Medicare. Typical treatment of just spider veins is considered a cosmetic treatment and therefore insurance companies will not cover the treatment. At the time of your consultation, the doctor will determine if your vein treatment is cosmetic or medically necessary. Consult your local insurance provider to determine your exact eligibility and coverage as well as cost.
Q: What are venous stasis ulcers?
A: A skin ulcer, caused by a venous reflux disorder is called a venous stasis ulcer. It is an irregularly shaped wound with well-defined borders, surrounded by red or dark and thickened skin. Venous ulcers vary in size and location, but are usually found on the inside of the lower leg.